What ıs the Gastric By-Pass Surgery
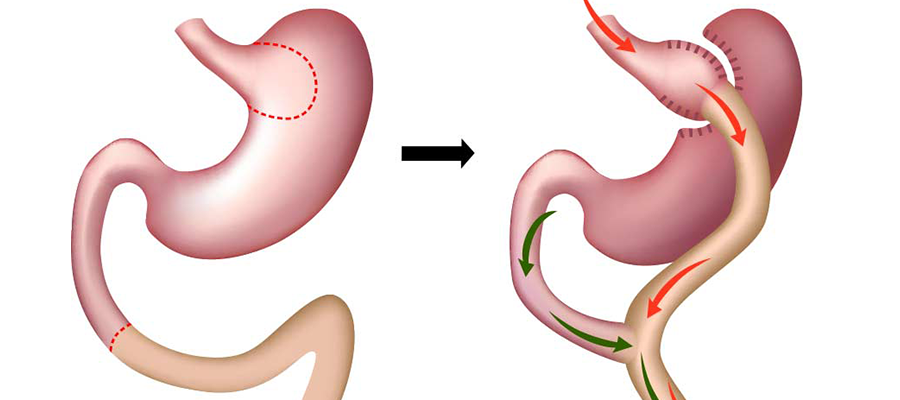
Gastric bypass surgery is a kind of bariatric surgery used to help patients lose weight by rearranging their digestive systems. Patients with severe obesity-related health issues who have not lost enough weight with diet, exercise, and medication are the usual candidates for this procedure.
The Roux-en-Y gastric bypass is the most popular of the several gastric bypass procedures available today.
The surgeon uses surgical staples to form a tiny pouch at the top of the stomach. Only the contents of this bag will be digested. This implies that less food is needed to achieve the same satiety levels as previously.
The surgeon next makes an incision in the small intestine and sews a section of it onto the pouch. The next section of the intestine will receive food from the pouch. Bypassing the stomach and the first portion of the small intestine (duodenum) is what gives this procedure its name, “gastric bypass.”
The smaller stomach causes the individual to eat less.
The tiny intestine absorbs less calories and nutrients.
Changes in hormone levels that cause one to feel full and eat less.
Extreme and permanent weight reduction.
The stomach’s capacity for food intake is limited.
Can result in a dramatic lowering or elimination of obesity-related health issues such type 2 diabetes, high blood pressure, sleep apnea, and lipid abnormalities.
Complications and Threats that May Occur
Infections, hemorrhages, clots, and breathing problems are all examples of potential short-term consequences.
Too rapid emptying of the stomach into the small intestine causes a condition known as “dumping syndrome.” Nausea, vomiting, abdominal distention, diarrhea, lightheadedness, and profuse perspiration may result.
Reduced nutrient absorption, leading to nutritional deficits. This might be a chronic problem that necessitates taking vitamins and minerals for the rest of your life.
Impaction of the bowels.
Irritation of the stomach lining, which may lead to ulcers or heartburn.
The possibility of a hernia forming at the incision site.
Failure to lose weight or gain back the weight lost.
What do they remove during gastric bypass?
The most frequent kind of gastric bypass surgery involves making structural changes to the digestive tract (without actually removing anything from the body). What happens throughout the operation is as follows:
A tiny pouch is created by using surgical staples to split the upper portion of the stomach from the remainder of the stomach. This bag, roughly the size of an egg, is inadequate for even a modest meal.
The surgeon performs a small intestinal bypass by first severing the intestine into two halves. The newly formed stomach pouch is joined directly to the bottom portion of the small intestine. By doing so, the first section of the small intestine (the duodenum) and a good chunk of the second part (the jejunum) are avoided.
After the top part of the small intestine (which was bypassed) is linked to the lower part of the intestine, the procedure is complete. This permits the meal to be mixed with the digestive fluids generated by the stomach and duodenum, which were skipped.
Food will avoid the majority of the stomach, the whole duodenum, and a portion of the jejunum as a consequence of the re-routing of digestive juices. Because of this, less calories and nutrients are absorbed by the body.
Is gastric bypass good or bad?
Significant Weight Loss: Many people who undergo gastric bypass experience substantial weight loss, often losing 60-80% of their excess body weight within the first year or two after surgery.
Improvement in Comorbidities: Conditions like type 2 diabetes, hypertension, sleep apnea, and certain cholesterol abnormalities can be significantly improved or even resolved following the surgery.
Increased Longevity: Some studies have shown that individuals who undergo bariatric surgery have a reduced risk of death compared to obese individuals who do not have the surgery.
Quality of Life: Many people report improved quality of life after surgery, including better mobility, self-esteem, and overall mood.
Hormonal Changes: Gastric bypass can lead to changes in gut hormones that reduce appetite, increase satiety, and enhance insulin sensitivity.
Cons of Gastric Bypass
Surgical Risks: As with any surgery, there are risks associated with anesthesia, infections, blood clots, and other immediate post-operative complications.
Dumping Syndrome: This condition occurs when food moves from the stomach into the small bowel too quickly, leading to symptoms like nausea, vomiting, bloating, diarrhea, dizziness, and sweating.
Nutritional Deficiencies: Because the surgery alters the digestive system, there can be reduced absorption of nutrients, leading to deficiencies that might require lifelong supplementation.
Chronic Issues: Some patients may experience long-term issues like bowel obstructions, hernias, ulcers, or low blood sugar.
Weight Regain: While less common with gastric bypass than with other types of bariatric surgeries, some people might regain some of the weight they lost.
Mental Health Challenges: Rapid weight loss can lead to emotional and psychological challenges. Some individuals might face issues with body image, depression, or anxiety after the surgery.
Irreversibility: While some bariatric procedures can be reversed, the gastric bypass is generally considered permanent.
Do you still have a stomach after gastric bypass?
Yes, after gastric bypass surgery, you still have your stomach. However, the surgery drastically changes how your stomach functions. Here’s what happens:
Creation of a Small Pouch: During the Roux-en-Y gastric bypass (the most common type), the surgeon creates a small pouch from the top part of the stomach using surgical staples. This small pouch is typically about the size of an egg.
Bypassing the Rest of the Stomach: The rest of the stomach remains in place, but it is bypassed. This means that food no longer goes into this part of the stomach when you eat.
Rerouting the Small Intestine: The small intestine is then rearranged so that it connects to the newly created stomach pouch, allowing food to bypass the larger part of the stomach and the first segment of the small intestine.
The larger, bypassed portion of the stomach still produces digestive juices, which are rerouted further down the small intestine to aid in digestion.
Why is gastric bypass good?
Gastric bypass surgery has several advantages, particularly for individuals with obesity and related health conditions. Here are some of the primary reasons why gastric bypass is considered beneficial:
Significant Weight Loss: Gastric bypass typically results in a substantial reduction in body weight. On average, patients can expect to lose about 60-80% of their excess body weight within the first year or two after surgery.
Resolution or Improvement of Comorbidities: Gastric bypass can lead to the improvement or even resolution of obesity-related health conditions, such as:
Type 2 diabetes: Many patients experience significant improvements in blood sugar control or even remission of their diabetes.
Hypertension: Blood pressure often normalizes or is significantly reduced.
Sleep apnea: Weight loss can lead to improvement or resolution of sleep apnea.
Hyperlipidemia: There’s often an improvement in cholesterol and triglyceride levels.
Joint pain and osteoarthritis: Weight loss can reduce stress on joints, alleviating pain and discomfort.
Increased Life Expectancy: Some studies have shown that the overall risk of death is lower for individuals who undergo bariatric surgery compared to those with severe obesity who do not.
Enhanced Quality of Life: Many individuals report an improved quality of life after surgery. This improvement encompasses physical activities, self-esteem, social interactions, and mental health.
Hormonal and Metabolic Benefits: Gastric bypass induces changes in gut hormones that promote satiety, suppress hunger, and may even enhance metabolic rate. It can also lead to improved insulin sensitivity, benefiting those with type 2 diabetes.
Sustained Weight Loss: Compared to other weight loss methods and some other bariatric surgeries, many people who undergo gastric bypass tend to maintain a more significant portion of their weight loss long-term.
Decreased Cardiovascular Risk: The surgery leads to improvements in cardiovascular health markers, decreasing the risk of coronary heart disease, stroke, and peripheral heart diseases.
Reduction in Cancer Risk: Some studies suggest that bariatric surgeries, including gastric bypass, may lead to a reduced risk of certain cancers, especially those associated with obesity.
What are the side effects of gastric bypass?
Short-term and long-term risks and side effects are associated with gastric bypass, as is the case with any surgical treatment. In some people, no or very few adverse effects are experienced, while others may have a number of problems. Some of the possible negative outcomes of gastric bypass include the following:
Bleeding, infection, blood clots, and negative responses to anesthesia are all examples of potential complications during surgery.
Surgical sites have a risk of leaking, which may cause infections and abscesses in the digestive system.
Strictures: Narrowing at the point where the intestines are linked, which may need medical intervention.
Consequences and dangers over the long term:
When food, particularly sugar, is emptied from the stomach into the small intestine at an abnormally rapid rate, a condition known as “dumping syndrome” may develop. Nausea, vomiting, diarrhea, lightheadedness, and profuse perspiration are some of the symptoms.
Deficiencies in nutrients occur when a section of the small intestine is skipped or the stomach is too small. Vitamin B12, iron, calcium, and vitamin D deficiency are just a few examples of how this might affect your health.
Scar tissue from the operation has the potential to develop bowel obstruction.
A hernia is a protrusion of tissue through an abdominal wall, and it is possible for one to form near the surgical incision.
Ulcers of the stomach and small intestine are possible.
Rapid weight loss may cause gallstones, which can be treated or even lead to removal of the gallbladder.
Some individuals have low blood sugar (hypoglycemia) after eating, a condition known as “reactive hypoglycemia.”
Stomal stenosis, or a narrowing of the passage between the stomach and intestines, may lead to nausea, vomiting, and abdominal pain.
Depression, anxiety, and body dysmorphia are just a few of the mental health issues that may arise as a result of drastic changes in body image, the stress of fast weight loss, and the difficulty of adapting to new eating and living patterns.
Additional sources of worry
Some people who lose weight may put it back on if they don’t stick to the advised diet and exercise plan.
Many individuals report increased sensitivity to alcohol after surgery. It’s absorbed rapidly and has a higher potential for rapid intoxication.
Who needs gastric bypass surgery?
The primary target population for gastric bypass surgery consists of very obese people who have failed to lose weight using more conservative methods. Gastric bypass surgery is a major procedure, and the choice to have it done should be made after careful consideration and discussion with the patient’s healthcare team.
In most cases, people who have gastric bypass surgery have at least two of the following conditions:
Guidelines based on Body Mass Index
The body mass index (BMI) of 40 or above. If a person weighs over 100 pounds beyond their ideal weight for their height, they are considered morbidly obese.
A body mass index (BMI) between 35 and 39.9, with a substantial obesity-related health concern (comorbidity), such as type 2 diabetes, hypertension, or severe sleep apnea.
Previous Attempts at Weight Reduction: Over a long length of time, the person has attempted to shed pounds by diet and exercise, but to no avail.
The patient is fully aware of the procedure’s potential dangers, advantages, and long-term effects. They are determined to permanently alter their diet, workout routine, and other lifestyle habits. This entails doing things like keeping your follow-up visits, taking your vitamins, and eating the way your doctor recommends.
The absence of medical issues that might enhance the risks of surgery or be made worse by it rules out surgery as a treatment option.
Candidates should have a psychiatric examination done to see whether they can handle the drastic lifestyle, eating, and self-perception changes that would be necessary after surgery. Postoperative compliance may be difficult in cases of untreated or unstable mental health issues, which are screened for during this examination.
While there is no hard and fast age limit for gastric bypass surgery, the associated risks do rise with advancing years. It’s important to assess the pros and cons, particularly for older individuals and younger teens.
Lack of Substance Abuse Issues: Addiction to drugs or alcohol may make it difficult to recover properly after surgery and follow post-op instructions, so it’s best to rule out substance abuse before scheduling surgery.
Obesity may be caused by or make weight reduction more difficult for those who also suffer from endocrine diseases like Cushing’s syndrome, if it is not under control. Before contemplating surgery, these conditions must be addressed and controlled.